Our vision
We are an EU-funded medical consortium that studies the connections between gut microbiota, diet, and exercise to formulate nutrition and lifestyle recommendations for brain health.
We are an EU-funded medical consortium that studies the connections between gut microbiota, diet, and exercise to formulate nutrition and lifestyle recommendations for brain health.
Follow the educational talks imparted by out Eat2beNICE experts!
Watch the latest talk by Dr. Alejandro Arias Vásquez on the link between the gut and the brain.
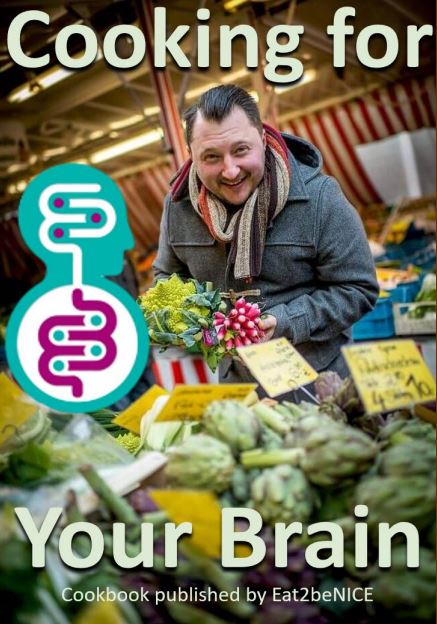
Follow the Celebrity Chef and Nutritionist Sebastian Lege for nutritional tips and recipes to live a healthier life, both mentally and physically.
New Online Cook Book available